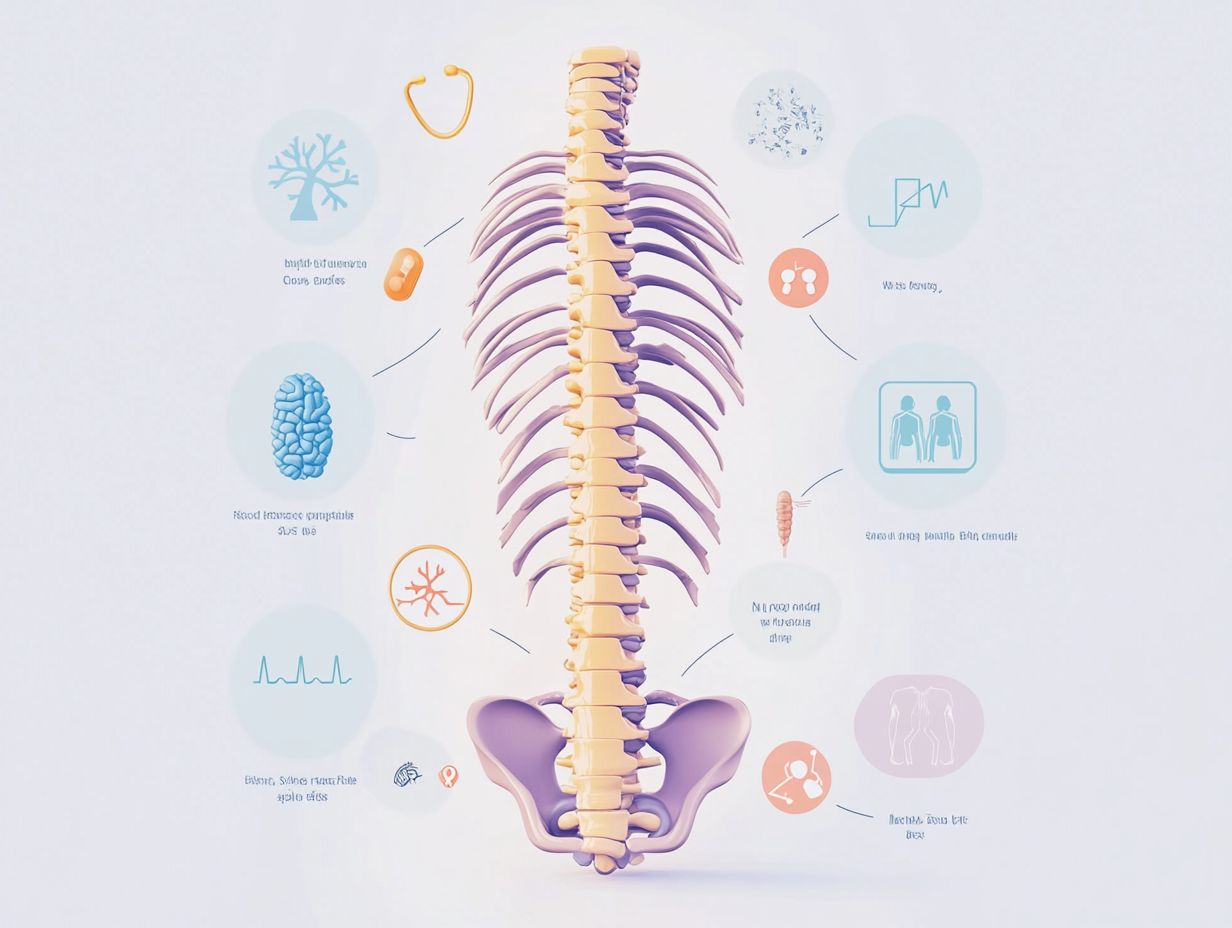
Understanding Spinal Stenosis: Causes and Treatments
Spinal stenosis is a condition that affects many individuals, often leading to discomfort and reduced mobility.
Understanding its causes, symptoms, and available treatment options is vital for anyone navigating this diagnosis.
This article explores what spinal stenosis is, how prevalent it is, and the various factors that contribute to its development.
It also discusses effective management strategies and provides insight into living with this condition.
Join us as we uncover everything you need to know about spinal stenosis.
Overview of Spinal Stenosis

Spinal stenosis is a medical condition defined by the narrowing of the spinal canal, which may exert pressure on the spinal cord and nerve roots. This pressure can lead to back pain and a range of other debilitating symptoms.
What is spinal stenosis?
Spinal stenosis is defined as the narrowing of the spinal canal, which affects the spinal cord and nerve roots, leading to a variety of symptoms, most notably back pain.
This condition can significantly impact an individual’s quality of life, as the reduction in space within the spinal canal may result in the compression of vital structures. The causes of spinal stenosis frequently include age-related changes such as osteoarthritis, congenital factors, herniated discs, or prior injuries that may alter the anatomy of the spine.
As the spaces within the spine narrow, individuals may encounter symptoms that range from radiating pain, numbness, and tingling to weakness in the limbs. These symptoms can worsen with specific activities and may result in mobility challenges.
It is essential to recognize the importance of early diagnosis and treatment, as timely interventions can help prevent further complications and improve the overall well-being of those affected.
How common is spinal stenosis?
Spinal stenosis is a prevalent condition, particularly among individuals aged 50 and older, with a substantial proportion experiencing back pain associated with this diagnosis.
This narrowing of the spinal canal can impact individuals across various age groups; however, it is more commonly observed in older adults due to the natural degeneration of the spine over time. Factors such as degenerative changes, which occur as the intervertebral discs and joints lose hydration and elasticity, as well as the presence of osteoarthritis, significantly contribute to the development of spinal stenosis.
Additionally, individuals who have suffered spinal injuries or possess a hereditary predisposition to spinal conditions may be at an elevated risk for developing this painful disorder.
Timely identification and management of spinal stenosis can help alleviate symptoms and enhance overall quality of life.
Symptoms of Spinal Stenosis
The symptoms of spinal stenosis can present with considerable variability; however, they frequently encompass back pain, numbness, and weakness in the extremities. These symptoms typically arise as a result of spinal cord compression and pressure on the nerve roots.
What are the symptoms of spinal stenosis?
Common symptoms of spinal stenosis include back pain, numbness, weakness in the legs or arms, and difficulty walking, all of which result from pressure on the spinal cord and nerve roots.
These manifestations can vary significantly depending on the location of the stenosis, whether in the lumbar or cervical region. In cases of lumbar stenosis, individuals may experience radiating pain down the legs, which often worsens with prolonged standing or walking, a condition referred to as neurogenic claudication. Conversely, cervical stenosis may present symptoms such as tingling, numbness, or weakness in the arms and hands, frequently accompanied by neck pain.
Early recognition of these symptoms is essential, as prompt diagnosis and treatment can prevent further complications and enhance mobility, ultimately improving the quality of life for affected individuals.
Causes of Spinal Stenosis
The causes of spinal stenosis can be multifactorial, encompassing age-related degenerative changes, arthritis, congenital spinal stenosis, and spinal injuries. Each of these factors contributes to the narrowing of the spinal canal.
What causes spinal stenosis?
Spinal stenosis can arise from a variety of factors, including degenerative changes in the spine, arthritis, and prior spinal injuries that contribute to the narrowing of the spinal canal.
As individuals age, the intervertebral discs may experience a loss of hydration and elasticity, leading to a reduction in disc height and an increase in vertebral encroachment. Osteoarthritis plays a significant role in the development of spinal stenosis by facilitating the formation of bone spurs, which can extend into the spinal canal and compress nearby nerves.
This narrowing can result in considerable pain and discomfort, ultimately limiting mobility and adversely affecting overall quality of life. Additionally, prior spinal injuries may lead to inflammation, scar tissue formation, or misalignment, which can further exacerbate existing conditions and create additional complications regarding the structure and function of the spinal column.
Aging and age-related changes in the spine
Aging naturally induces degenerative changes in the spine, characterized by the thickening of ligaments and the formation of bone spurs, both of which can contribute to spinal stenosis and the narrowing of the spinal canal.
As individuals progress in age, these changes may become more pronounced, often leading to the compression of spinal nerves and surrounding tissues. Conditions such as osteoarthritis, which are prevalent among older adults, can exacerbate these issues by promoting inflammation and joint degeneration. This deterioration not only diminishes flexibility but may also result in pain and a reduction in mobility.
Additionally, as the intervertebral discs lose hydration and elasticity, they may shrink, contributing to spinal instability. This further narrows the spinal canal and increases the associated risks of spinal stenosis.
Arthritis and other conditions
Arthritis, particularly osteoarthritis, is a significant contributor to the development of spinal stenosis, as it induces inflammation and degeneration of the spinal joints, leading to the narrowing of the spinal canal.
This condition often results in increased pressure on the spinal cord and nerve roots, thereby exacerbating symptoms such as pain, numbness, or weakness in the extremities. As the joints continue to deteriorate, the formation of bone spurs may occur, further compromising the already limited space within the spinal canal. The inflammatory processes associated with arthritis can also intensify existing pain, creating a detrimental cycle that hinders mobility.
For individuals affected by these conditions, understanding the relationship between arthritis and spinal stenosis is crucial for effective management and relief.
Inherited conditions
Certain inherited conditions may result in congenital spinal stenosis, characterized by a narrower spinal canal from birth, which increases the likelihood of experiencing back pain and other related symptoms in later life.
These conditions may encompass factors such as skeletal dysplasia, which can affect the development of bone and cartilage, leading to vertebrae that assume a shape contributing to spinal canal narrowing. Additionally, some individuals may inherit genes that predispose them to conditions such as achondroplasia or scoliosis, both of which can significantly influence the narrowing of the spinal canal over time.
Understanding these genetic factors is essential, as early diagnosis and intervention can markedly enhance the quality of life for affected individuals, facilitating effective symptom management and the prevention of further complications.
Diagnosis and Tests for Spinal Stenosis
Diagnosing spinal stenosis generally requires a comprehensive review of the patient’s medical history, a detailed physical examination, and the use of various imaging tests. These steps are essential for evaluating the spinal canal and identifying any obstructions or degenerative changes that may be present.
How is spinal stenosis diagnosed?

The diagnosis of spinal stenosis involves a comprehensive approach that includes a thorough physical examination and advanced imaging techniques such as MRI and CT scans. These methods are essential for visualizing the spinal canal and assessing any narrowing that may be present.
These evaluations are critical in identifying the underlying causes of symptoms such as pain, numbness, or weakness in the limbs. During the physical examination, the healthcare provider assesses the patient’s posture, flexibility, and strength, while also checking for any signs of nerve impairment.
Subsequently, MRI scans provide detailed images of soft tissues, including the spinal cord and nerve roots, facilitating the precise detection of stenosis. Additionally, CT scans can be employed to examine bony structures and confirm any abnormalities that may contribute to the condition.
Collectively, these diagnostic tools are integral to developing a comprehensive understanding of the individual’s spinal health and informing subsequent treatment options.
Management and Treatment Options
Management and treatment options for spinal stenosis are diverse and may encompass both non-surgical interventions, such as physical therapy and pain management techniques, as well as surgical procedures when deemed necessary.
What are the treatment options for spinal stenosis?
Treatment options for spinal stenosis encompass a spectrum ranging from conservative approaches, such as physical therapy and anti-inflammatory medications, to more invasive surgical procedures designed to alleviate symptoms and restore functionality.
The selection of a treatment strategy typically depends on the severity of the symptoms, the overall health of the patient, and the extent of spinal canal narrowing. For example, physical therapy is aimed at strengthening core muscles, enhancing flexibility, and improving posture, and is frequently recommended for individuals with mild to moderate stenosis.
Anti-inflammatory medications serve to manage pain and swelling, offering temporary relief for patients who may not be prepared for more aggressive interventions. In cases where patients experience severe pain or neurological symptoms, minimally invasive treatments such as epidural steroid injections can provide significant alleviation of discomfort.
When conservative treatments prove ineffective, surgical interventions, including decompression surgery or laminectomy, present viable options that can lead to substantial improvement, particularly for patients exhibiting progressive symptoms or considerable impairment.
Non-surgical treatments
Non-surgical treatments for spinal stenosis encompass a variety of approaches, including physical therapy, pain management strategies such as anti-inflammatory medications, and epidural injections, all aimed at alleviating symptoms without necessitating surgical intervention.
These methods are designed to enhance mobility, reduce inflammation, and improve overall quality of life, thereby enabling individuals to engage in daily activities with greater ease.
Physical therapy specifically targets the strengthening of muscles that support the spine, providing tailored exercise regimens that enhance flexibility and diminish pain. Concurrently, medications play a crucial role in addressing inflammation and discomfort, offering relief that allows patients to participate in therapeutic activities.
Epidural injections, which are administered directly into the epidural space, provide targeted pain relief through the delivery of steroids that can significantly mitigate symptoms. Collectively, these non-invasive options constitute a comprehensive pain relief strategy for individuals suffering from spinal stenosis.
Surgical options
In instances where non-surgical treatments prove ineffective, surgical options for spinal stenosis may be evaluated, including decompression surgery and spinal fusion, each presenting its own set of risks and benefits.
These surgical procedures are designed to alleviate pressure on the spinal cord and nerves, thereby enhancing the patient’s quality of life. Decompression surgery entails the removal of bone spurs or ligaments that contribute to the narrowing of the spinal canal, while spinal fusion aims to stabilize the spine by fusing two or more vertebrae.
Indications for these surgical interventions typically include severe pain, notable mobility impairments, and neurological deficits that adversely affect daily activities. The prognosis following surgery is generally favorable, with many individuals experiencing significant relief from symptoms; however, outcomes may vary based on the extent of nerve damage and the patient’s overall health.
Therefore, it is essential for patients to engage in thorough discussions regarding potential risks and rehabilitation strategies with their healthcare provider.
Prevention of Spinal Stenosis
Although spinal stenosis cannot always be prevented, it is possible to significantly reduce the risk factors associated with its development by maintaining a healthy spine.
This can be achieved through regular exercise, proper body mechanics, and avoiding spinal injuries.
Can spinal stenosis be prevented?

While complete prevention of spinal stenosis may not be feasible, several proactive measures can be implemented to maintain a healthy spine and reduce the risk of its development.
Engaging in regular physical activity is essential, as it strengthens the muscles that support the spine and enhances overall flexibility. Incorporating low-impact exercises, such as swimming or walking, can be particularly advantageous for individuals aiming to maintain joint health.
Additionally, managing body weight is crucial, as excess weight can impose additional pressure on the spine, thereby exacerbating the risk factors associated with stenosis. Furthermore, posture correction should be emphasized, as proper alignment during daily activities can significantly alleviate strain on the spine and promote long-term spinal health.
Prognosis and Outlook
The prognosis for spinal stenosis is influenced by multiple factors, including the severity of the condition, the efficacy of treatment options, and the overall health of the individual. These factors can vary significantly from one patient to another.
What is the prognosis for spinal stenosis?
The prognosis for spinal stenosis can vary significantly among patients. While many individuals experience substantial pain relief and enhanced functionality through conservative treatment options, others may require surgical intervention and encounter a more complex recovery process.
This variability is influenced by several factors, including the patient’s age, overall health status, and adherence to the treatment recommendations provided by healthcare professionals. Generally, younger individuals tend to recover more swiftly and effectively compared to older adults, who may experience additional challenges due to comorbidities.
Maintaining good overall health through lifestyle choices, such as a balanced diet and regular exercise, is crucial for facilitating recovery. Compliance with treatment regimens, which may include physical therapy, medications, and regular follow-up appointments, is essential for achieving optimal outcomes.
Patients who actively engage with their healthcare teams and prioritize their treatment plans are more likely to experience favorable results.
Living with Spinal Stenosis
Living with spinal stenosis presents considerable challenges, particularly in managing symptoms such as back pain and sustaining an active lifestyle. This condition requires continuous communication with a healthcare provider to develop and implement effective treatment strategies.
When should I see my healthcare provider about spinal stenosis?
Individuals experiencing symptoms of spinal stenosis, such as persistent back pain, numbness, or weakness, should promptly consult their healthcare provider to discuss diagnostic and management options.
It is imperative for those affected to recognize that additional concerning signs, including difficult walking, loss of bladder or bowel control, or sudden changes in mobility, require immediate medical evaluation. These symptoms may indicate significant compression of the spinal cord, which could result in permanent damage if not addressed without delay.
Early intervention by healthcare professionals is essential, as it not only aids in diagnosing the underlying issues but also provides individuals with appropriate treatment plans, potentially preventing further deterioration of their condition. Timely care is critical in enhancing quality of life and restoring mobility, ensuring that patients can manage their symptoms effectively.
